Oral Appliance Exercises
IN BRIEF A Summary of the Optimal Use Project Treating Obstructive Sleep Apnea
Key Messages
- Tailor the treatment of obstructive sleep apnea (OSA) based on a patient’s disease severity and other patient factors.
- Treatment of mild OSA may not be needed. Lifestyle modifications for patients who are overweight or obese may be effective.
- Treat moderate to severe OSA with continuous positive airway pressure (CPAP). If CPAP is not acceptable, treat with oral appliances.
- Consider surgery for OSA only if other treatments have failed or are unacceptable.
Context
Obstructive sleep apnea (OSA) is a sleep disorder that affects
as many as one in four adults in Canada. When people with OSA fall asleep, the muscles in their throats relax, causing their upper airways to collapse. As a result, their breathing stops and restarts throughout the night. Symptoms of OSA include snoring, unrefreshing sleep, excessive daytime sleepiness, lack of concentration, impaired memory, and lower quality of life. Anyone can develop OSA, but some factors may increase the risk, such as obesity, male gender, older age, alcohol and drug use, smoking, having narrowed airways, and family history. Untreated, OSA can lead to serious health complications such as fatigue, hypertension, cardiovascular events, and diabetes. Across Canada, OSA leads to a substantial economic and societal burden.
Technology
There are many available treatments for OSA:
- Continuous positive airway pressure (CPAP) forces air into the upper airway to prevent the soft tissues from collapsing ― and is often considered the gold standard of OSA treatment.
- Other positive airway pressure (PAP) devices such as auto-titrating PAP (APAP) and bilevel PAP (BiPAP) are also available.
- Nasal expiratory PAP (EPAP) valves are disposable devices that use a patient’s own breathing to create positive pressure in the airways at the end of a breath to prevent airway collapse.
- Oral appliances (OAs) include mandibular advancement devices (MADs) that bring the jaw forward to maintain an open airway, and tongue-retaining devices (TRDs).
- Surgery, called maxillomandibular advancement (MMA), permanently pulls the lower jaw forward to create more space and prevent airway collapse.
- Another type of surgery called genial tubercle advancement (GTA) removes bone tissue from the chin and pulls the base of the tongue forward to create more airway space. It may be performed along with MMA.
- Other possible treatments include positional therapy, as well as lifestyle interventions such as diet and exercise to help patients with OSA who are obese or overweight to lose weight.
Issue
With so many treatment options available for OSA, deciding which intervention is best suited to each patient can be difficult. Public coverage of the costs of these treatments varies across Canada, leading to differences in access for Canadians. Providing a review of the evidence and expert recommendations on the treatment of OSA will help clinicians, policy-makers, and patients to best use available OSA treatment options in Canada.
Methods
In Brief: Treating Obstructive Sleep Apnea To address the issue of OSA treatment in Canada, CADTH undertook an Optimal Use project to assess the clinical and cost- effectiveness, safety, and patient experiences of interventions for OSA in adults. Ethical issues, implementation considerations, and the potential environmental impact were also addressed. The Health Technology Expert Review Panel (HTERP) developed recommendations for treating OSA based on the evidence.
Results
For the clinical overview of systematic reviews (SRs), meta- analyses, and health technology assessments (HTAs), 33 SRs were included. For the supplementary review of primary studies for areas of gap, 41 primary studies were included. CPAP, EPAP, MADs, TRDs, MMA, GTA, weight loss programs, and positional
therapy were all effective at reducing excessive daytime sleepiness and OSA severity, compared with inactive controls or pre-treatment. For excessive daytime sleepiness as the outcome, effect sizes were similar across the interventions, except for people with severe cases of OSA who may benefit more from CPAP than from MADs. For OSA severity as the outcome, effect sizes varied across the interventions, with CPAP showing the largest effect, followed by EPAP, and then MADs or OAs. For people with severe cases of OSA who are eligible for surgery, MMA with or without GTA may be effective at improving both excessive daytime sleepiness and OSA severity.
Cost-effectiveness of treatment strategies for OSA was found to
be dependent on a patient’s baseline OSA severity (as measured
by the Apnea–Hypopnea Index or AHI). At a willingness-to-
pay threshold of $50,000/quality-adjusted life-year (QALY), the
order in which interventions were considered cost-effective by
increasing disease severity were: no treatment (AHI < 15), MADs
(15 ≤ AHI ≤ 25), MMA with or without GTA (25 < AHI < 30), PAP
therapy (30 ≤ AHI ≤ 32), and MMA with or without GTA (AHI>32).
The patient experiences review revealed that a range of
characteristics and factors influence whether people seek and
initiate OSA treatment, including their prior expectations and
beliefs about treatment, the social support they have available,
and their lifestyles. The review also revealed that interventions
for OSA require people to adapt their daily routines and
relationships, and that some people are able to integrate the
interventions into their lives and experience benefits, while
others are unable to do so.
The review of ethical issues revealed six key values: respect individual autonomy, maximize benefits and minimize harms for patients, maximize benefits and minimize harms for others affected by OSA, maximize benefits and minimize harms for populations, distribute benefits and burdens of health care resources fairly, and steward scarce resources.
One of the biggest implementation issues found was the difficulties
in accessing sleep specialists and sleep labs to obtain a diagnosis,
if appropriate, and begin to seek appropriate treatment. Barriers
for CPAP included cost and patient discomfort, while supports
included patient education and ongoing support. OA barriers
included lack of physician awareness, dental health requirements,
and the need for regular re-evaluations.
Little evidence on the environmental impact of OSA treatment was identified. One study was found which focused on the manufacturer adoption of green packaging, as well as energy- efficient and recyclable devices.
Read more about the CADTH OSA project:
www.cadth.ca/OSA
Questions or comments about CADTH or this In Brief?
Learn more: cadth.ca
Contact us: [email protected]
Follow us on Twitter: @CADTH_ACMTS
Subscribe to our E-Alert and New at CADTH newsletter: cadth.ca/subscribe
Disclaimer
The information in this document is intended to help health care decision-makers, patients, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. This information should not be used as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process nor is it intended to replace professional medical advice. While The Canadian Agency for Drugs and Technologies in Health (CADTH) has taken care in the preparation of this document to ensure that its contents are accurate, complete, and up-to-date, CADTH does not make any guarantee to that effect. CADTH is not responsible for any errors or omissions or injury, loss, or damage arising from or as a result of the use (or misuse) of any information contained in or implied by the information in this document.
CADTH takes sole responsibility for the final form and content of this document. The views expressed herein are those of CADTH and do not necessarily reflect the views of our funders.
ABOUT CADTH
CADTH is an independent, not-for-profit organization responsible for providing Canada’s health care decision-makers with objective evidence to help make informed decisions about the optimal use of drugs and medical devices in our health care system.
CADTH receives funding from Canada’s federal, provincial, and territorial governments, with the exception of Quebec.
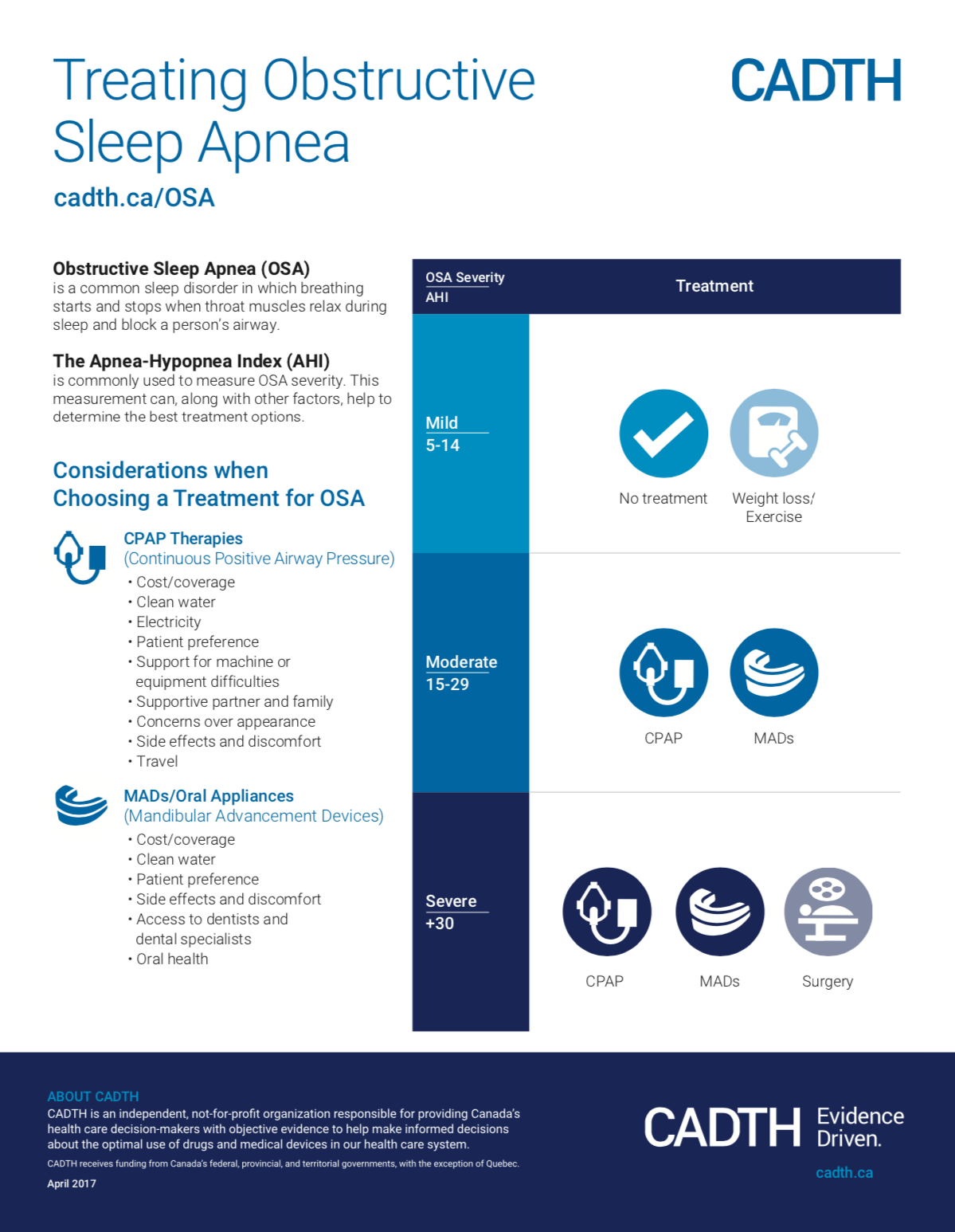
Treating Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA)
is a common sleep disorder in which breathing starts and stops when throat muscles relax during sleep and block a person’s airway.
The Apnea-Hypopnea Index (AHI)
is commonly used to measure OSA severity. This measurement can, along with other factors, help to determine the best treatment options.
Considerations when Choosing a Treatment for OS
CPAP Therapies
(Continuous Positive Airway Pressure)
• Cost/coverage
• Clean water
• Electricity
• Patient preference
• Support for machine or equipment difficulties
• Supportive partner and family
• Concerns over appearance
• Side effects and discomfort
• Travel
MADs/Oral Appliances
(Mandibular Advancement Devices)
• Cost/coverage
• Clean water
• Patient preference
• Side effects and discomfort • Access to dentists and dental specialists
• Oral health
Article on “Patient preferences and experiences of CPAP and oral appliances for the treatment of obstructive sleep apnea: a qualitative analysis
Sleep apnea is a common chronic disease and the treatments available require the patients to use it every night. Recently, medicine has improved their focus on chronic disease management, and has given better focus on the patient experiences to improve the long-term benefits of treatments. This article points out the main experiences and preferences from individuals who have used CPAP or Oral Appliance or both. It is really interesting for patients deciding on the treatment to read the table 3, on page 662.
Given that there is a choice of treatments, this study illustrates that despite negative aspects of both treatments, such as discomfort, noise of machine, bite changes for example, patients were still committed to using a sleep apnea treatment.
Recognizing a patient’s willingness to improve their symptoms and respecting their choice of treatment helps the practitioner and patient to select the best treatment to meet their physical and lifestyle needs.
Prediction in obstructive sleep apnoea: diagnosis, comorbidity risk, and treatment outcomes
This review article where Dr. Almeida is one of the co-authors is an interesting overview of obstructive sleep apnea. It covers the areas of P4 medicine, which is currently being used more and more in various areas. The four P’s stands for prediction (risk one person has to develop sleep apnea); prevention (risk prevention strategies); personalized (addressing individual needs and specific characteristics); and participation (getting patient involvement in their own care).
Important risk factors known to be associated with sleep apnea are obesity (general and localized), smaller jaws and or head features and neuromuscular control. As the last one we are starting to better understand, obesity is an important factor to pay attention to. Some studies suggest that 10% of weight loss can lead to about a 30% decrease in the apneas at night.
In term of symptoms, not everyone feels the same as a result of the decrease breathing at night. Some individuals develops sleepiness, others develop insomnia while up to 30% could feel completely normal (asymptomatic). A very important are of research today, with unfortunate not many answers, is the understanding on who will develop problems because of sleep apnea. There is consensus that moderate to severe patients have higher chances, but not everyone will have them.
This article further describes treatments such as CPAP, oral appliance, weight loss, surgeries and some new approaches which are still under testing for a promising improved care for all patients in the future.
https://www.tandfonline.com/doi/abs/10.1080/17476348.2018.1439743
CADTH REPORT
Interventions for Sleep Apnea
This is a very nice summary, focused on optimum use of treatments for sleep apnea. Dr Almeida has served as a consultant for CADTH in the literature review and analysis. Documents from CADTH are often used by policy makers to approve provincial health coverage for treatment. In this article, they pointed out that for moderate to severe OSA, CPAP, oral appliances and maxilla-mandibular surgery are cost-effective treatment, meaning the provider is saving money on possible future health complication if they pay for any of these treatments instead of leaving patients untreated.
It is important to tailor the treatment to each patient, which should involve the severity of the disease as well as patients factors such as preference and access to dentist specialized in the field.
https://www.cadth.ca/interventions-obstructive-sleep-apnea
https://cadth.ca/sites/default/files/pdf/CADTH_OSA_Infographic-e.pdf